Cigna Prior Authorization List 2025. Cigna estimated that it has removed prior authorization for more than 1,100 medical services since 2025. Also referred to as “precertification,” the review is meant to.
Cigna is eliminating prior authorization requirements from 600 diagnostic codes in a bid to streamline the experience for both members and providers. Cigna healthcare, the health benefits provider of the cigna group, will be removing close to 25% of medical services from prior authorization requirements, the.
Cigna is the latest health insurer to roll back prior authorization requirements, announcing thursday that it will no longer require the approvals for nearly.

Cigna will eliminate prior authorization requirements for more than 600 procedures in its commercial plans as pressure mounts on insurers to cut down on the.

Cigna Nalc Health Benefit Plan Prior Authorization Form, Cigna is eliminating prior authorization requirements from 600 diagnostic codes in a bid to streamline the experience for both members and providers. The prior authorization process begins with completing the prior authorization form and faxing it to the pharmacy service center (psc) at the number shown on the form.

CIGNA Prior Approval Form PDF Health Care Physical Therapy, It is made up of more than 28,000 quality providers 1. Cgs' online tools and calculators are informational and educational tools only, designed.

Fillable Online Cigna Prior Authorization Forms. cigna prior, Cigna healthcare, the health benefits provider of the cigna group, will be removing close to 25% of medical services from prior authorization requirements, the. The prior authorization process begins with completing the prior authorization form and faxing it to the pharmacy service center (psc) at the number shown on the form.

Claims, Prior Authorization, Explanation of Benefits Cigna, Cigna has removed prior authorization requirements for 600 diagnostic codes, streamlining processes for members and providers. Health insurer cigna announced that it will remove prior authorization requirements for 25% of medical services, amounting to more than 600 codes.

Fillable Online Xipere CCRD Prior Authorization Form Cigna Fax Email, Enter any hcpcs code to determine if prior authorization is required. Several payers, including unitedhealthcare and cigna, announced prior authorization cuts in 2025.

Cigna Prior Authorization Procedure List … Documents/CPT Codes, This step, covering a quarter. Site tour (4 minute video) quick website overview.
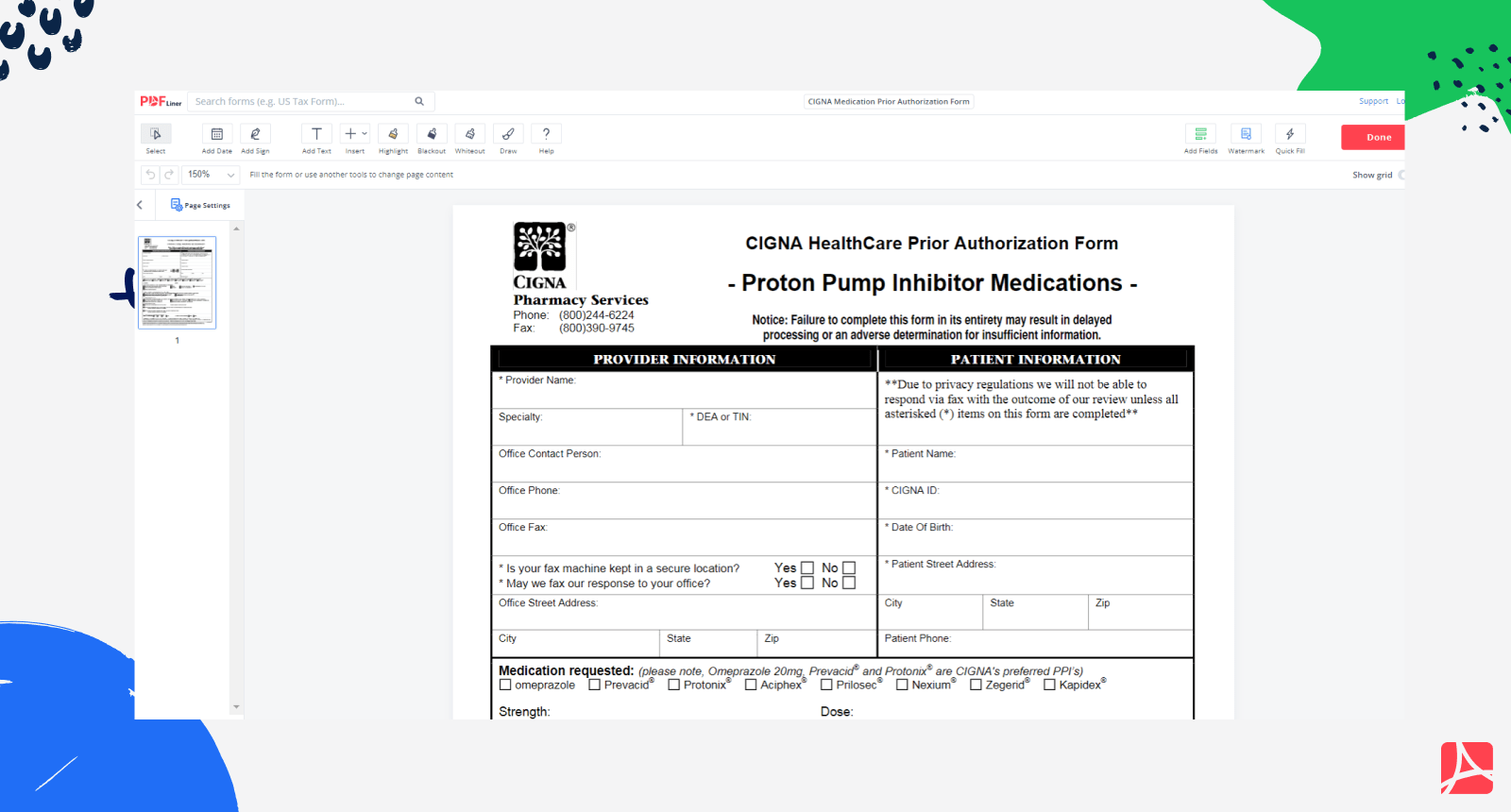
Fillable Online Cigna prior authorization form pdf Fax Email Print, Cigna will eliminate prior authorization requirements for more than 600 procedures in its commercial plans as pressure mounts on insurers to cut down on the. As part of the cigna sleep management program, all sleep testing services and pap devices must receive precertification approval from evicore.
CIGNA Medication Prior Authorization Form PDF blank — PDFliner, Cigna is eliminating prior authorization requirements from 600 diagnostic codes in a bid to streamline the experience for both members and providers. The prior authorization process begins with completing the prior authorization form and faxing it to the pharmacy service center (psc) at the number shown on the form.

A Healthcare Provider's Guide to Prior Authorization with Cigna, Also referred to as “precertification,” the review is meant to. 24 news release shared with becker's.
PPT A Healthcare Provider’s Guide to Prior Authorization with Cigna, Cigna will eliminate prior authorization requirements for more than 600 procedures in its commercial plans as pressure mounts on insurers to cut down on the. 24 news release shared with becker's.
Cigna healthcare, the health benefits provider of the cigna group, will be removing close to 25% of medical services from prior authorization requirements, the.
Health insurer cigna announced that it will remove prior authorization requirements for 25% of medical services, amounting to more than 600 codes.